Does this sound like you?
1. 57-year-old male is experiencing right hip pain that is affecting his quality of life and simple day to day activities. X-rays revealed that the cause of his pain is mild to moderate osteoarthritis. He has been diligent with physiotherapy for several weeks, which has been helpful, but he feels that recently he has stopped making progress. Tylenol and Advil offer only temporary improvement in his symptoms.
2. 36-year-old female has recently taken up tennis. It is also a busy time at her job where she does a lot of computer work. She has noticed the gradual development of pain over the outside of her elbow that is worse with grip. Despite rest, bracing, and the appropriate physiotherapy, her symptoms have persisted for 5 months.
3. 45-year-old male developed knee swelling a day after an intense bout of exercise. Despite rest and ice, the swelling has persisted and is affecting his ability to walk and sleep. He is in too much pain to participate in physiotherapy.

All of the individuals described in the above scenarios could benefit from an ultrasound guided injection/procedure by a skilled physician. This blog is an overview of the basics of ultrasound guided injections and how they can be used to help manage musculoskeletal injuries such as osteoarthritis and tendinopathy (a chronic tendon injury) – see if they apply to you!
What is Ultrasound and why do we use it?
- Ultrasound is a powerful and portable clinical/real-time imaging tool
- Safe for everyone (no radiation)
- It can be helpful in diagnosing a problem
- Research has shown that injections done under ultrasound guidance are also more accurate when done by a skilled practitioner, which in turn also means they have a higher likelihood of being effective
What would make me a good injection candidate?
- Osteoarthritis
- Tendinopathy (like tennis elbow, shoulder or gluteal tendinopathy)
- Adhesive Capsulitis (Frozen Shoulder)
- Baker’s cysts
- Ganglion cysts
- Carpal Tunnel Syndrome
- de Quervain’s tenosynovitis
- Trigger finger
- Bursitis (shoulder, hip, etc.)
What would make me a good injection candidate?
Ultrasound guided injections can be considered in many different scenarios. For example, you could consider undergoing an ultrasound guided injection/procedure if you:
- Are unable to tolerate participation in physiotherapy due to high pain levels
- Have poor sleep quality due to pain despite other efforts
- Have plateaued in your progress with physiotherapy/other conservative strategies
- Need additional diagnostic clarity (diagnostic injections), for example, in surgical planning
- Need to manage your symptoms as you await surgery
What kind of injection is best for me?
This is an important conversation to have with your Sports Medicine doctor. They can assess your injury, including the type, severity, etc., and review the pros and cons to each injection type so that you can come to an informed decision together. In the summaries below, you can review the basics about each of the ultrasound guided injection options that are offered at our clinic.
Types of Injections
CORTISONE
What is it? “Cortisone” is a corticosteroid (hormone), a strong anti-inflammatory.
Who can benefit from it? An acutely painful musculoskeletal condition, such as an arthritic/swollen joint can benefit from a cortisone injection.
How quickly does it work? Typically within 2 days – 2 weeks.
How long does it last? Average duration is 6-12 weeks (results vary).
What are the pros? Fast acting, inexpensive, strong anti-inflammatory properties.
What are the cons? Shorter duration of efficacy on average, can cause damage to cartilage and tendons in the long term (more likely with more exposure), higher risk in people with poor bone health (e.g. osteoporosis).

HYALURONIC ACID (Viscosupplement/”lubricant”)
What is it? A synthetic version of a molecule that is present in our natural joint fluid; acts as a lubricant and “shock absorber”, helps reduce pain/inflammation and improve function.
Who can benefit from it? People with mild-moderate pain related to a mild-moderately osteoarthritic joint.
How quickly does it work? Typically within 2-4 weeks.
How long does it last? An average of 6 months.
What are the pros? Not damaging to cartilage, lasts longer on average compared to cortisone, tends to be covered by supplemental insurance plans.
What are the cons? Takes longer than cortisone to start working, higher cost than cortisone (if no supplemental insurance).
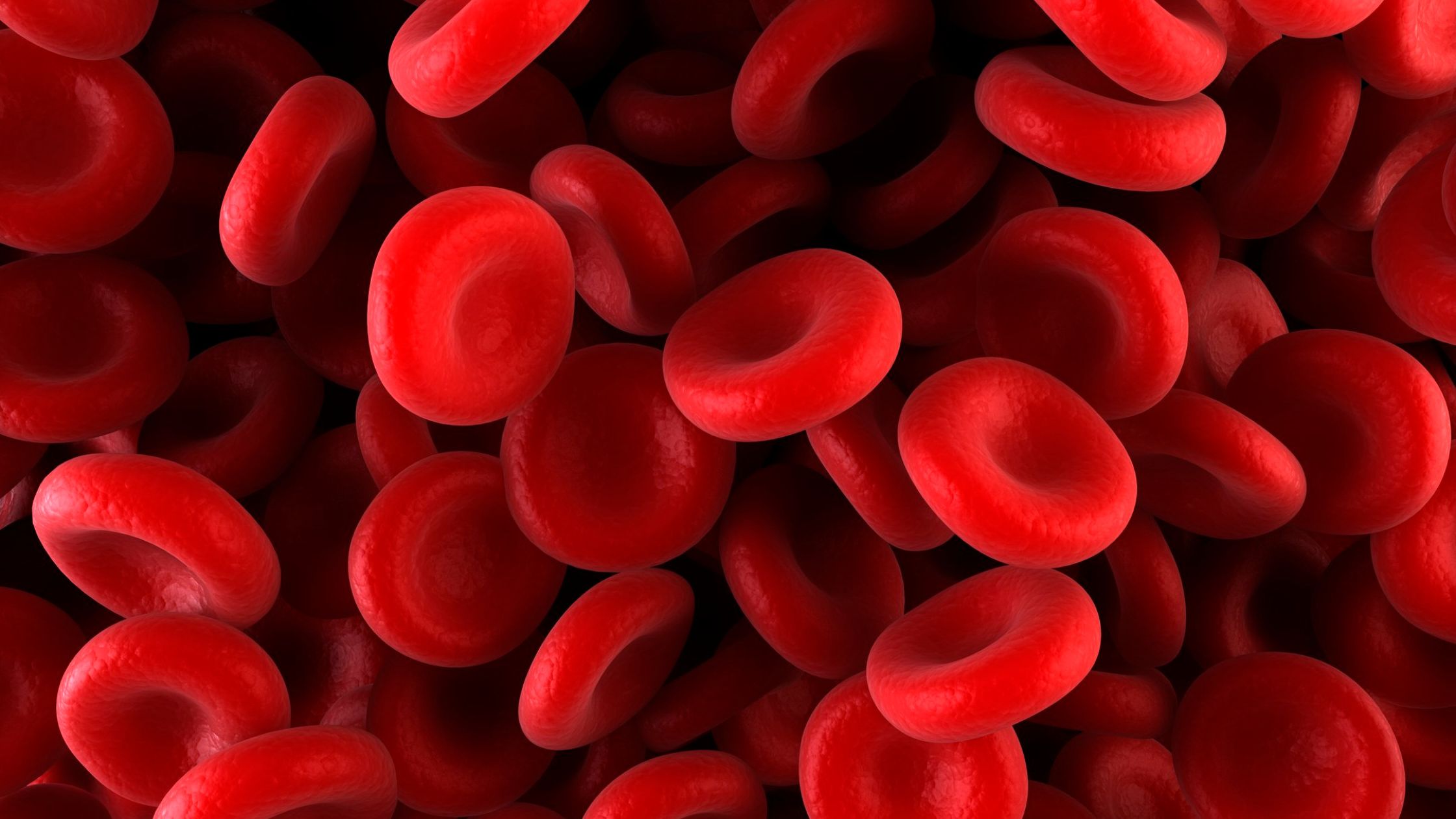
PLATELET RICH PLASMA (PRP)
What is it? From a small sample of your own blood, your platelets (a type of blood cell) are concentrated and injected into the damaged area (joint/tendon) to optimize the environment, protect cartilage and improve pain/function.
Who can benefit from it? People with mild-moderate pain related to a mild-moderately osteoarthritic joint, or chronic tendinopathies.
How quickly does it work? Joints can take 4-6 weeks to start feeling relief, tendons can take 6-10. Maximal improvement occurs over a 3-6 month period.
How long does it last? Average 12 months in mild to moderate OA; can be longer when treating certain tendinopathies, like tennis elbow and gluteal tendinopathy.
What are the pros? Natural/from your own cells, not harmful to tissue, works longer on average vs cortisone/hyaluronic acid available for tendons as well as joints.
What are the cons? Not covered by insurance (out of pocket expense), and can take longer to take effect vs cortisone.
nSTRIDE
What is it? From a small sample of your own blood, white blood cells and their “anti inflammatory proteins” (cytokines) are concentrated and injected into the arthritic joint, targeting the “inflammatory proteins” that contribute to cartilage breakdown.
Who can benefit from it? People with pain related to an osteoarthritic joint.
How quickly does it work? Substantial pain relief can begin 2-4 weeks after treatment, with maximal pain relief occurring between 8-12 weeks post treatment.
How long does it last? Average 1-2 years in mild-moderate osteoarthritis.
What are the pros? Natural/from your own cells, not harmful to tissue, works longer on average vs HA/CSI/PRP, specifically targets cartilage degradation in osteoarthritis.
What are the cons? Not covered by insurance (out of pocket expense), and can take longer to take effect vs cortisone.
Combining these injections with the appropriate rehab and post injection care is paramount in optimizing outcomes.
To be sure of which is right for you, it’s important to have a comprehensive evaluation by a Sports Medicine physician who is skillful in the use of ultrasound, and has knowledge of the clinical scenarios in which the use of these injections is appropriate.

